It’s been a few years, but when I think back on my doctor’s visits during pregnancy, the most vivid memories I have are of lying on the table and having my stomach measured. There was something so simple and physical about the idea that you’d just use a regular measuring tape, and somehow that would speak volumes. Having said that, I was never entirely sure what they were measuring or what they were getting from the measurements. Sometimes, in my less charitable moments, I wondered whether this was just a meaningless activity intended to convince me that the 45 minutes to an hour I’d just spent in the waiting room was worth it.
This measurement is called a “fundal height” measurement. Despite my grumpy feelings, it provides useful — if quite noisy — information about fetal growth. The other approach to estimating fetal size, more commonly used at the end of pregnancy, is ultrasound. With both of these metrics, there are natural questions about accuracy. If your belly is measuring big or small, how much do you learn from that? If the ultrasound says the baby is 10 pounds, are they? How sure can you be?
Unlike many of the topics I write about, this is one with a lot of good data. We can answer these questions. So let’s do it.
Fundal height measurements
The tape measure your OB is running over your belly is measuring fundal height — this is basically the size of the uterus measured from the top of the pubic area to the top of the uterus (that’s the “fundus”). The goal of measuring fundal height is to detect abnormal fetal growth, typically after 24 weeks.
To do this measurement, your doctor just … measures. The trick — and this is where the physical expertise comes in — is to be able to feel the points to measure between. Best practice is to measure using the unmarked side of the tape measure, to avoid bias. If we know what we are looking for, we may be biased to see it (this is why somehow many men seem to think they are 6 feet tall rather than, say, 5 foot 10. I digress).
After 24 weeks of pregnancy, the height of the fundus approximates gestational weeks. So it should be 26 centimeters around 26 weeks, etc. Data suggest a margin of error of plus or minus 3 centimeters, so within 3 centimeters of the expected number, we assume things are fine. If the measurement is 4 or more centimeters off what is expected, that’s a marker for possible fetal growth issues. The bigger concern is if the figure is much smaller than expected, which could be a sign of fetal growth restriction. Fetal growth restriction means the fetus is small, which could be a sign of a placental or other issue (or it could just be that they are small).
It is important to emphasize that phrase: could be a sign. It is a fairly crude approach to this — I say that in a positive, not a normative, way. There is information here, and it’s an easy test, so it’s impressive that we can get anything out of it! But you cannot make a diagnosis of growth restriction based on fundal height alone. This measurement is influenced by a variety of factors, including maternal weight, fibroids, whether you have to pee, if you drank a lot of water, and so on.
In terms of accuracy, there is a variety of data. One large study in Sweden used data from 42,000 women and asked whether small fundal height measurements were predictive of a baby being small for gestational age at birth. The researchers found that, in general, fundal heights were predictive, but much more so later in pregnancy. There are a few ways to summarize their results, but here is one take:
- If we take a measurement below the 10th percentile (a common threshold) as a cutoff to be concerned, about 25% of pregnant women will fall below this threshold at least once during their pregnancy.
- For 2 out of 10 “positive” findings on this test, the infant will be small for gestational age.
- For 9 out of 10 negative findings, the infant will not be small for gestational age.
The second bullet here might be the most relevant. For 8 out of 10 people who get a concerning result on this screen, they will have a normal-size baby. Again, this screening provides quite a lot of information, but it needs follow-up. You would not want to act, or panic, based on a worrisome result.
Typical follow-up if there is a concern with fundal measurement is an ultrasound to assess fetal growth. It is also common — even without any concern — to use an ultrasound to assess the fetus size near the end of pregnancy. How accurate are those? Let’s turn to that next.
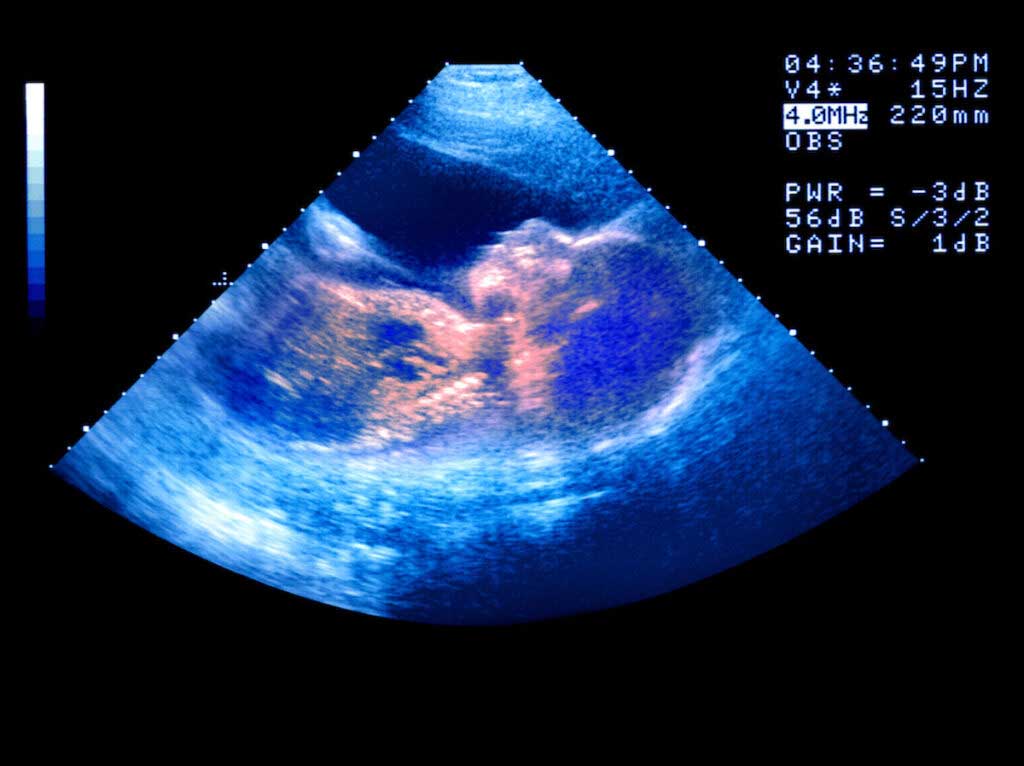
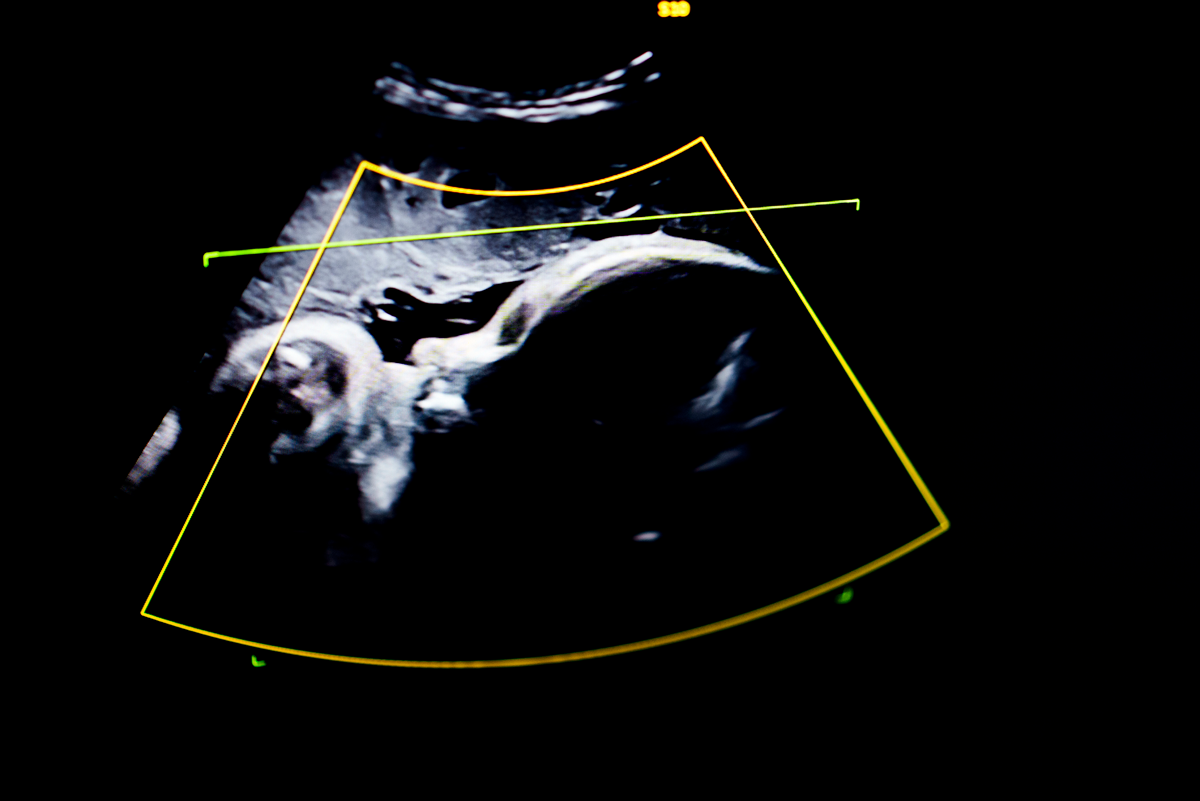
Measuring fetal size with ultrasound
The first thing to say here is that you cannot measure fetal weight directly with an ultrasound. What you can do with an ultrasound is take various body measurements. The main measurements used are head diameter, head circumference, abdominal circumference, and femur length. These can all be measured on an ultrasound, but with error. As you might imagine, reflecting on the circumstances of non-fetal humans, these measurements are not going to perfectly indicate weight. They’re likely to be a bit better with a fetus than an adult, for many reasons, but ultimately there is error.
The general system for estimating fetal weight involves taking these measurements, or a subset of them, and running them through a formula. These formulas are developed based on taking data on the measurements and then comparing them to actual fetal weight — researchers ask how they could combine the measurements to get the most accurate prediction.
There are many possible formulas that can be used and, to be frank, looking at them isn’t going to really help one understand anything. For example, here is a popular one (the “Hadlock three-parameter formula”):
EFW = 10(1.326 + 0.0107 × HC + 0.0438 × AC + 0.158 × FL − 0.00326 × AC × FL))
If you parse this, you see that estimated weight is increasing in head circumference (HC), abdominal circumference (AC), and femur length (FL), but also there is a downward adjustment for the interaction between femur length and abdominal circumference. The goal of these formulas isn’t to be interpretable, it’s to get the best fit to the data.
In practice, all of these formulas perform similarly, and all have the same problem. They are all pretty accurate on average. That is: if your question was what the size of the average baby is, these formulas do pretty well. This is more or less mechanical: these formulas are explicitly developed in a way that would make that true. But they all come with a lot of error. This is true for a few reasons. First, there is error in the measurements that are used as inputs — it’s not that easy to measure head circumference with ultrasound. Second, even if the measurements were perfect, there is variation across babies.
The size of the errors are pretty large. A 2023 study of more than 30,000 babies in Sweden looked at estimated weight on an ultrasound within two days before birth and compared it to actual birth weight. Between 70% and 75% of the fetuses had a birth weight within 10% of estimated. But this means that as many as 30% of the babies were over or under by at least 10%. That’s the difference between 7 pounds and 6 pounds 5 ounces, which is … big. As many as 6% of measurements were off by more than 20%, which renders them basically useless.
The errors are larger for very small and very large babies. This is not surprising, since there are less data on those, so the models have less information to fit to. It’s unfortunate, though, since those are precisely the situations in which these data are most useful. It actually isn’t that important to know if your baby is going to be 7 pounds 12 ounces or 8 pounds 6 ounces. When this matters more is if you’re expecting a very small baby (say, under 3 pounds) and want to know what to be prepared for, since 3 pounds and 2 pounds are very different, or if you’re expecting a very large baby, which might necessitate different delivery approaches.
There are various ways that the accuracy situation might be improved, including better measurements with 3-D ultrasound or MRI, and possibly better models. More data might allow better prediction at the end of the distributions, but maybe not. Ultimately, it’s a hard problem.
Given the large error, there are questions raised by some about whether these measurements should be taken at all. On one hand, more information is (usually) better, and there is clearly some information provided by these measurements. On the other hand, there are decisions made based on these data, and bad measurement may lead to clinical error.
For example: there is evidence that when fetal weight is overestimated, women are more likely to have a C-section for labor arrest. Put simply, if labor is slow, and the estimated fetal weight suggests the baby is big, doctors (in this study at least) were more likely to move to a C-section than with the same length of labor and the same actual size of baby but a higher estimated weight.
There’s no consensus here, unfortunately, and in most practices, estimating fetal weight near the end of pregnancy is standard. I should note that ultrasound is also used, and also has significant error, for detecting fetal growth restriction during pregnancy. The same problems that plague the estimation of weight near birth come up here. It is just not very precise.
Bottom line
- There are no precise methods for estimating fetal size in utero.
- Fundal measurements are simple to do, and provide a signal about growth, but the majority of concerns raised by these measurements are unfounded.
- Ultrasound-based measurements are accurate on average, but about 30% of people will have errors of more than 10% in either direction.
- For most people, these measurements never play a role in your care, so their lack of precision doesn’t matter. If you are asked to make decisions based on estimated fetal weight (for example, a decision about an induction or a C-section) consider asking for a second measurement.
















Log in