Ask Me Anything About “The Unexpected”

- Featured
- Most/Least Popular
- Newest/Oldest

- Babies
- Medical Care
Topic:General Discussions
Thread closing on
 ParentData
ParentData
6 days ago
Ask Me Anything About “The Unexpected”
Over the past two years, my co-author, Dr. Nathan Fox, and I wrote The Unexpected. It is a guide to navigating pregnancy during and after complications. Our hope is that it can be a starting point for normalizing discussions about these topics, so we can better support one another and provide further research and resources for birthing people everywhere.
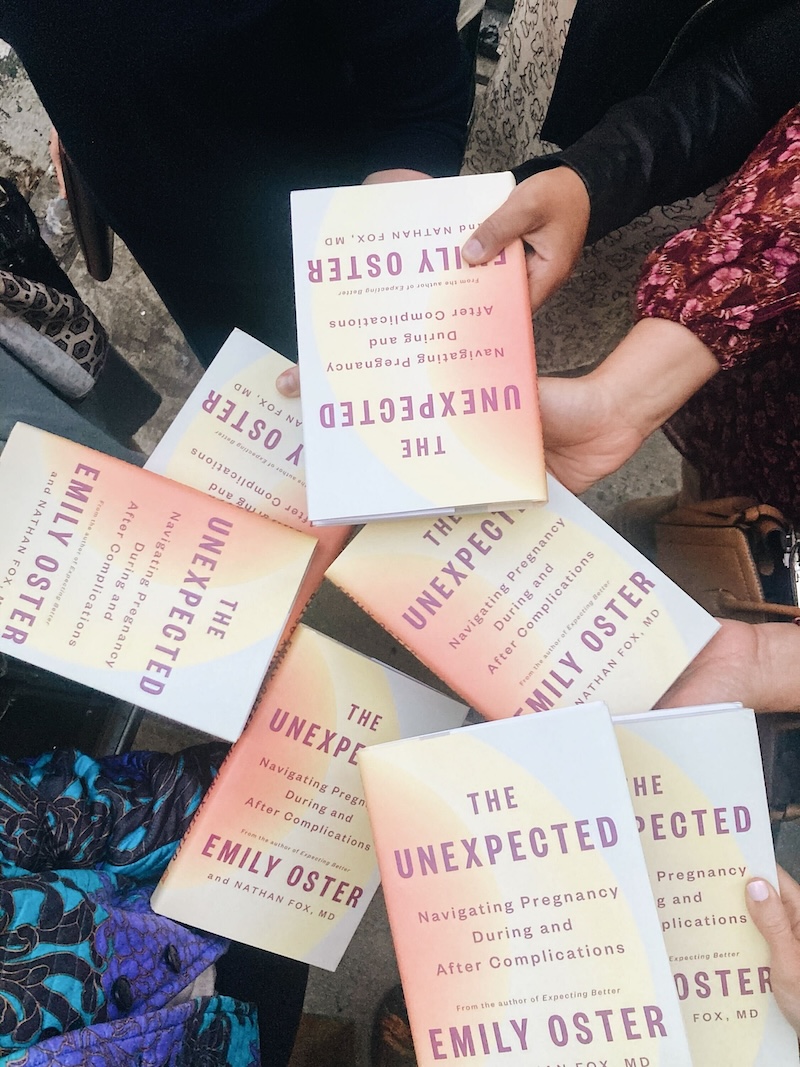
I’m excited to answer some of your questions about the book and hear what you think about it. I’ll be popping in to respond this weekend and throughout the week.
Alright, I’m ready for it. Ask me anything!
—Emily
- You must be logged in to reply to this topic.
Log in
-
6 days, 5 hours agoJoanna.r
I was diagnosed with vasa previa for my first pregnancy. I was on pelvic rest starting at week 20, admitted to the hospital at week 32 for constant monitoring, and delivered my daughter via c-section at week 35. (She’s 4 months old and doing great!) Should we be fortunate enough to get pregnant again, what’s the likelihood I’ll be diagnosed with vasa previa again?
2 comments-
5 days, 7 hours agokatherinepg
Almost identical timeline, and same question about Complete Placenta Previa and undiagnosed Placenta Accreta! Was able to keep my uterus.
0 comments -
5 days, 6 hours ago Emily Oster
Emily OsterVasa previa — where blood vessels from the umbilical cord grow in a way that is unprotected — can be very dangerous if not diagnosed. If it is diagnosed, a C-section (typically early — 34 to 35 weeks) is life-saving.
The good news is that this condition is almost always totally random, meaning your likelihood if being diagnosed with it again isn’t meaningfully elevated. And since the condition is rare, the risk is small.
0 comments
-
-
6 days, 5 hours agomaggiep
Do you discuss ECV/breech presentation in the book?
1 comments-
5 days, 9 hours ago Emily Oster
Emily OsterNot in this book — but there is a long discussion of this in Expecting Better and one here as well:
0 comments
-
-
6 days, 3 hours agoCEP410
Hi, do you discuss cholestasis (intrahepatic cholestasis of pregnancy) in the book?
2 comments-
6 days, 1 hour agoMegB
I don’t believe it is, but I experienced this condition (among others listed in the book) and would also love to hear more about any research or data associated with approaching this in another pregnancy-—how likely it it to reoccur and how should you approach early delivery? I felt so misinformed.
1 comments-
5 days, 9 hours ago Emily Oster
Emily OsterMeg is correct — it’s not in this book, although our hope is that the general discussion in the first part of the book would be helpful regardless of condition. We have this on a list of topics to consider adding to a later edition (and to ParentData).
0 comments
-
-
5 days, 20 hours agoZWxlYW5vci5tY2NhbGx1bUBnbWFpbC5jb20=
Not discussed and if you look it up on Dewey on this website it will tell you it’s “no risk to baby”. Pretty disappointing to see this from the ai bot on this on this website in particular. ICP tends to get overlooked.
0 comments
-
-
6 days, 3 hours agoMartha
Thank you so much for writing this. I survived 2/5 of the severe maternal morbidity chapter and as a bonus, the pre-eclampsia chapter, and the thing I have been wondering is how to compare the mortality risk of giving birth again to the mortality risks of things I do in my every day life. Given the probability of recurrence and the mortality risk of the types of complications I know I am at higher risk for, is my chance of dying if I have a second baby like my lifetime risk of dying in a car accident? Motorcycle? Sky-diving? (note: I do not do those last two things).
0 comments -
6 days, 3 hours agokgpalm
The chapter on miscarriage didn’t include low progesterone as a cause of miscarriage, but I have seen articles saying low progesterone causes miscarriage and progesterone supplementation can help prevent miscarriage in some cases. Is low progesterone not an evidence based cause of miscarriage? What are your thoughts on studies on progesterone supplementation?
3 comments-
5 days, 9 hours ago Emily Oster
Emily OsterWe discuss the evidence on progesterone in the context of preterm birth in that chapter. In the case of miscarriage, the data overall doesn’t provide strong support for a role of supplementation in preventing miscarriage. In the largest randomized trial of this treatment for recurrent pregnancy loss there was no impact on pregnancy rates or outcomes. Having said that, there are smaller trials or more specific ones that suggest there could be some small effect in some cases. This is a case with a lot of clinical disagreement about what the best course of action is.
0 comments -
5 days, 9 hours agokgpalm
Perhaps for a little context I will add, I was taking at home urine progesterone tests that showed I had low progesterone when I got pregnant, then at 6 weeks, I had a miscarriage. My ObGYN doesn’t want to test or treat for low progesterone after only one miscarriage. I’m wondering how much to push back and also how much to worry when I get pregnant again.
2 comments-
5 days, 8 hours agoLindsay M
My first pregnancy was a miscarriage, and I suspected low progesterone (I wasn’t testing at home like you were, but I did consistently have a 9-10 day luteal phase which made me suspect low progesterone). I was suspicious that the loss might be related to the low progesterone and convinced my doctor to prescribe progesterone supplements. My next conception was a successful pregnancy. However …
I started looking more into the research around progesterone supplementation and pregnancy loss, and I realized that it was not very convincing. If I remember correctly, there was a small effect only in women with 3 or more consecutive losses. When I started trying for my second child, I opted not to go on progesterone supplementation, and I was able to get pregnant just fine and it was not a loss.
This is all 100% anecdotal of course, but since I was in a similar situation as you I figured I’d share!
0 comments -
5 days, 4 hours agolndemery
With my last pregnancy, I tested for low progesterone and was ordered supplements by my doctor. My levels rose only slightly, but just want to caution that it made me so sick to the point I was suffering from dehydration.
0 comments
-
-
5 days, 3 hours agoJo
I’ve had low progesterone for all 3 of my pregnancies now (and one premature birth), so the discussions about the evidence are always of interest to me. I think there is ambiguous evidence in general, but there are also differences in oral supplementation vs. shots that probably require different research threads (ref. the controversy about Makena recently coming off the market).
Both OB practices I worked with are somewhat unusual in that they automatically test progesterone levels at the beginning of pregnancy and monitor throughout. I’m thankful, because my pregnancies do follow a pattern of labor being triggered almost immediately after progesterone supplemental ended. Even though the evidence for progesterone is mixed, I’m grateful that my providers view it as a low-risk intervention that can’t hurt, even if it doesn’t help. There are many women in my extended family who endured several miscarriages before this was an option, and I can’t help imagining how their lives could have been so dramatically different with a fairly simple hormone supplement.
I’m also fascinated by related theories about vitamin D supplementation preventing preterm birth. Is there any more research on this than progesterone?
0 comments
-
-
6 days, 1 hour agoLFH
Hi
Is there anything in the book about unexplained preterm babies (I had a total healthy normal pregnancy but waters broke at 35 weeks, no reason has been suggested by any medical professional) and likelihood of this happening again?
It’s a serious consideration of mine when deciding whether or not we should have another.
Thanks2 comments-
5 days, 9 hours ago Emily Oster
Emily OsterYes — in the chapter on preterm birth we talk through the recurrence risks and also possible explanations. On average, for women who deliver a first baby between 32 and 36 weeks, there is about a 15% chance of a preterm birth in a second pregnancy. This is an average — the recurrence risk is lower if there is an avoidable reason for the preterm birth (like infection) and possibly higher if there is a systematic reason.
If you do pursue another pregnancy, it’s certainly a good idea to talk to your doctor in advance to see if you can understand anything more about why this happened in your case, and what treatments might be available.
0 comments -
5 days, 7 hours agoBirdyk
I had this happen as well at 36 weeks. My doctor has said that there’s no way to know why my water broke early (PPROM) even though I wonder if it was because I exercised the two days before consecutively even though I exercised regularly through the pregnancy. I do know there was no infection when they ran tests. When I brought up progesterone she said it doesn’t work. I feel pretty anxious and uncertain about what, if anything to do or try this second time around and worried that it will happen again but maybe earlier? When you say 15% chance of it happening again, can you explain that in relation to other things we do day to day that have this risk?
0 comments
-
-
6 days agoTbolibol
I bought the book and read it after experiencing two miscarriages within the last 6 months. Confirmed uterine septum so hoping to get that fixed soon. One thing I was really hoping to find in the book was information about miscarriages and how they are handled. The first time I went through a miscarriage the process was so confusing and you have to make choices on how to proceed. Do you want to try to pass it naturally? Take medication? Receive a D&C? I would love hear your perspective on the data out there about the risks and pros of each of these options.
1 comments-
5 days, 6 hours ago Emily Oster
Emily OsterI’m sorry this wasn’t in the book! It’s covered more extensively in Expecting Better and I wrote about it long-form here. https://elemental.medium.com/what-to-expect-when-you-have-a-miscarriage-74114d2bb7de
The choices here are absolutely complex and — like many complications — there is a lot of personal preference. A D&C is the fastest way to complete a miscarriage, but many women prefer to manage miscarriage at home. Taking medication works in about 80% of cases, with 20% needing a subsequent D&C. In the end, these are all safe options — if incredibly hard — and talking through what you want with your doctor is crucial.
0 comments
-
-
5 days, 18 hours agokim90x
I just had an emergency c-section delivery (at term) because of a placenta abruption. I’d like to have another child, but I’m not sure what risks I now have of that happening again. How are pregnancies after placenta abruption handled?
1 comments-
5 days, 9 hours ago Emily Oster
Emily OsterThe answer here depends a little bit on why you had the abruption. Sometimes, a placental abruption is clearly due to an event like a car accident. In that case, there is not much reason to worry about recurrence. If the abruption was unexplained, then your doctor may want to watch you more carefully. This would likely mean more visits, especially towards the end of pregnancy, and probably a planned C-section or induction at 39 weeks.
0 comments
-
-
5 days, 18 hours agoLaurenKnight
Does The Unexpected cover molar pregnancy? Currently on the long road to recovery from this difficult but rare pregnancy complication.
1 comments-
2 days, 11 hours agoSunnyDays76
I also had a molar pregnancy (partial molar) and am curious about this too. I’m not sure if you’ve had another child or pregnancy before, but for me it was my first pregnancy and very challenging trying to interpret the data and risks after. That said, I ended up trying again (after I was cleared) and had 2 healthy pregnancies after!
0 comments
-
-
5 days, 9 hours ago sunnysurfer
sunnysurferIs there any way to see data on severe maternal morbidity by hospital system and how it’s trending over time? We talk a lot about how women can make birth safer through self advocacy but I want to see what hospitals are doing to address this too— especially when choosing where to give birth.
1 comments-
5 days, 9 hours ago Emily Oster
Emily OsterThis is a great question. The short answer is that this data isn’t available in any systematic public way. Researchers are sometimes able to get this for particular hospitals or systems, but there isn’t a public reporting system.
You CAN ask at the hospitals you are considering, or ask related questions — C-section rate, for example. A caution is that hospitals that treat a higher risk population of patients will seem to have “worse” outcomes, even if they are better hospitals overall.
0 comments
-
-
5 days, 9 hours agoTaylorL
A dear friend of mine has a bicornate uterus, which makes her more prone to pregnancy loss and complications. As she begins her conception journey, how can I be prepared to support her as a friend? How can I balance helping her prepare for potential loss while, at the same time, rejoicing in the possibility of a baby?
1 comments-
5 days, 8 hours ago Emily Oster
Emily OsterAsk her! This question is so personal, and everyone’s approach is going to be different. But the simple question: “How can I best support you in this journey?” is going to give you a lot of what you need to know. Holding onto joy while living with the possibility of grief is among the hardest things.
0 comments
-
-
5 days, 9 hours agoHayley
Thank you so much for writing this book!! Looking forward to reading it soon. My question is- does the book go into detail about how to prevent certain complications moving forward? I had gestational hypertension and postpartum hemorrhage and would love to know if I could decrease my risk for either of those with the next pregnancy. Thank you again!!
1 comments-
5 days, 9 hours ago Emily Oster
Emily OsterYes! The structure of the second part of the book is to discuss specific conditions, and then go into the risk of recurrence and possible treatment options (along with a discussion of how to talk to your doctor about your options)
0 comments
-
-
5 days, 8 hours agoEmily K.
I had a d&c two weeks ago for an early missed miscarriage (the embryo stopped growing at 6+3). I know the evidence suggests not waiting to try again after an early miscarriage, but I can’t find any data at all about d&c specifically. My ob says to wait one or two cycles to let the uterine lining regrow, but also says she is old fashioned and hasn’t really explained what the risk of getting pregnant before my period would be–higher risk of chemical pregnancy or miscarriage? Higher risk of ectopic? Nothing? It seems like the advice people get on this subject is all over the map. I don’t want to rush and cause more issues, but I’m 39 and the clock is ticking.Is there just really no data here?
1 comments-
5 days, 6 hours ago Emily Oster
Emily OsterThe advice to wait to conceive after a miscarriage is largely about dating a pregnancy. Since pregnancy dating is traditionally done based on your last period, if you do not have one between pregnancies it is harder to date them. Having said this, there are many other ways to date a pregnancy so it is not clear how important this is. There is no evidence to suggest that these pregnancies would be less viable or more likely to miscarry.
1 comments-
5 days, 4 hours agoEmily K.
Thanks! But I am wondering if this is equally true after a d&c as after a natural or medicine-induced miscarriage. There seem to be some doctors who believe the scraping of the uterine lining would leave it too thin to support a healthy pregnancy. Is there any data to support that idea?
1 comments -
5 days, 3 hours ago Emily Oster
Emily OsterI have not seen any data to suggest this, and since D&C is a common first trimester approach (and the uterine lining builds up and departs each month) it seems likely many of the cases covered in the studies would have had a D&C.
1 comments -
5 days, 2 hours agoEmily K.
Thanks so much! This is very useful.
0 comments
-
-
-
5 days, 8 hours agoelmonj
Do you think your research and findings/conclusions is relevant to both maternity care models- obstetrical and midwifery care? Did you come across any differences between the two? Curious if you pull in experts from both fields.
1 comments-
5 days, 3 hours ago Emily Oster
Emily OsterBecause we are talking about more complicated pregnancies, in most cases a midwife isn’t likely to be a good option for care. We do, however, talk at the top of the book about how to choose a provider, whether you might want to switch providers between pregnancies, and the possibility of a Maternal Fetal Medicine Specialist (like Nate is) instead of an OB.
0 comments
-
-
5 days, 8 hours agoRCM21
Does the book discuss any postpartum medical conditions that were triggered by pregnancy? I developed an autoimmune disease 4 months postpartum, and according to a few doctors I’ve met with, pregnancy can actually trigger autoimmune diseases and I might not have developed one in absence of pregnancy. Do you have any data on the incidence of this, and the likelihood of another pregnancy worsening my now preexisting autoimmune disease?
1 comments-
5 days, 6 hours agoalba.a
I was worried I had an autoimmune disease prior to getting pregnant and they tested my blood and did see something that was dormant. Can’t remember what it was and they did warn me it could develop from having a baby. So far nothing, but someone good to know in case it did activate something.
0 comments
-
-
5 days, 8 hours agomiriam0911
I’m definitely buying this! I had a near perfect pregnancy and delivery experience until I had a nerve injury during delivery. I had test after test done to see if it was epidural related or other nerve injury as I couldn’t walk because I had a foot drop. As I had all these women checking up on me some of them mentioned they had or knew someone who had experienced the same thing. The thing that struck me the most is they all acted like it was no big deal and it was just a thing that happened but I had never heard of it?! Do you discuss what “random” things can happen overall? The risk is “low” but is it?
1 comments-
5 days, 7 hours agoLindsay M
The foot drop thing happened to me too! During both of my deliveries! Both times I had an epidural, and both times I lost dosiflexion in my feet and could barely walk after. It was more severe with my first delivery, and pretty mild in my second. I was told that it’s not a direct result of the epidural, but more that during labor you might spend an extended amount of time in a position that compresses a nerve but not realize it because you have an epidural.
The first time it happened it was terrifying because no one could tell me if it was going to be a permanent complication or just a short term annoyance. It ended up getting 100% better within a few weeks. And the second time within only a few days.
0 comments
-
-
5 days, 8 hours agomommabear
The book mentions postpartum hemorrhage and uterine atony as a leading cause. what (if anything) can be done to lower this risk? Also, is it possible for PPH requiring blood transfusion to be caused by both uterine atony and retained placental products or another cause? Anything that can be done to lower risk of retained placental products? Asking as a pregnant mom with prior PPH. Thanks and thank you for this book!
1 comments-
5 days, 6 hours ago Emily Oster
Emily OsterUterine atony — when the muscles of the uterus are weaker and do not contract enough after birth — can interact with other conditions which cause bleeding. So the short answer is: yes, PPH could be caused by retained placental products exacerbated by uterine atony.
Uterine atony typically will recur in a later pregnancy but treatment is better if you expect it — more pitocin after birth to encourage contraction, for example. Retained placental product is more common is you’ve had multiple C-sections, although it is often unpredictable. Unfortunately, there is relatively little that can be done before delivery to prevent it.
0 comments
-
-
5 days, 8 hours agoLindsay M
I was diagnosed with severe postpartum preeclampsia 3 days after giving birth and re-admitted to the hospital after having initially been discharged. I did not have any high blood pressure during pregnancy at all. Does the book include information specifically on postpartum preeclampsia?
Also, I know with preeclampsia in general, the long term risk for CVD is higher. And yet, in the 6 years since my preeclampsia, no doctors have ever proactively suggested any kind of extra testing or screening and when I bring it up, they’re not sure what to say and there doesn’t seem to be any standard recommendation that I can refer to. Does the book talk about how the increased long term risk after pregnancy complications like preeclampsia should be handled?
1 comments-
5 days, 6 hours ago Emily Oster
Emily OsterYes — for both gestational diabetes and pre-eclampsia, these experiences can be kind of a window into future health. It’s not necessarily the case that pregnancy causes a higher risk, but that the stress on your body during pregnancy surfaces some issues which you are higher risk for.
There isn’t anything particular to do about this OTHER THAN to have your doctor be aware of your pregnancy history. If you have the same doctor, that’s easy, but it’s something to talk about with a new provider if you have one.
Dr. Gillian actually wrote about this in Hot Flash last week! https://parentdata.org/health-after-pregnancy-complications/
0 comments
-
-
5 days, 8 hours agotlh290
My 4 yr old had to have a CT scan of his abdomen and drink the dye- even though e we asked before and were told no another doctor did tell us after the surgery an ultrasound could have been done instead. Are his chances of developing cancer because of the radiation significantly higher?
0 comments -
5 days, 7 hours agoAlexis5656
Do you discuss or have you encountered pulmonary embolism during labor? Would love to find any other(s) who have experienced this!
0 comments -
5 days, 7 hours agocleverett1
I had a completely normal first pregnancy all the way until the end when they thought I had an induction failure but still ended up being able to deliver. My second pregnancy had structural complications (HRHS) and we terminated because of the incredible limited data about quality of life for this population. My main question is about subsequent pregnancies and how to manage the stress of wondering about all the things that could go wrong. Is there any research about preventing critical chd’s? Anything that could possibly help. Long time fan, thank you so much.
1 comments-
4 days, 2 hours agohec0903
I’m so sorry to hear about your second pregnancy, I can’t imagine what an incredibly difficult decision that had to have been to make.
I’m also curious about the risk of subsequent critical CHDs. I had a healthy pregnancy with no indication of structural abnormalities, and it wasn’t until our son’s 4 month checkup that our ped heard a previously undetected heart murmur. He was then diagnosed with ToF, and underwent OHS at 5.5 mo. We are so grateful for his incredible cardiology team, and he is now 13 months old and thriving, but as we think more about expanding our family, the thought of having another baby with a complex CHD (or any CHD, for that matter!) feels very intimidating. We’re in the process of having a genetic panel done for our son to see if there are any genetic markers that could explain his condition, but the likeliest scenario is that it was random. We’ve heard the chance of having a baby with a CHD is about 1%, but that it goes up to 5% if you’ve previously had a child with CHD. Is this accurate? We were also shocked that our son’s wasn’t detected in utero—his VSD was quite significant. What are the odds of critical CHDs going undetected in utero? I guess my question boils down to: how scared should we be going forward? I know that’s probably not easily answered. Just curious what the current data is!
0 comments
-
-
5 days, 7 hours agoelizlyle
Hi Emily! I’m curious if you and Dr. Fox studied the research on SPD. I had it with both pregnancies, and with my second, it was pretty extreme and debilitating – I was using a walker to get to the bathroom at night, for example. (Interestingly, the morning after delivering, I was like a new person after months of declining mobility and pain – it was unbelievable.) My doula described it like this: “SPD is to pelvic girdle pain as hyperemesis is to morning sickness”, which did a LOT to make me feel seen and understood. And miraculously my L&D nurse was 35 weeks pregnant herself (hero) and suffering from SPD, too, so she was able to help me navigate the delivery process and help the medical team to help me with being extremely careful in all the subtle ways that matter with SPD. Anyway, my question is: do you have any research on SPD, and particularly whether one should expect it to happen again if it’s happened before? We are likely to forgo having a 3rd simply because of SPD and how hard it was on my body and our family as a result. So it’s a big question on our minds!
0 comments -
5 days, 7 hours agonadiam
Does the book touch on risks/benefits and choosing between a vaginal birth and planned c section after a previous traumatic (ie. third degree tearing) vaginal birth? Specifically risk of repeat tearing and pelvic floor complications such and urinary incontinence and prolapse.
1 comments-
5 days, 3 hours ago Emily Oster
Emily OsterWe do talk about this, yes. Both about the risks of tearing, the risks of future complications, and how to have a conversation about consider a C-sectoin in these cases.
0 comments
-
-
5 days, 7 hours agoCarolineN
How concerned should I be about the long term impacts of preeclampsia, such as increased risk of heart disease?
0 comments -
5 days, 7 hours ago KateAndula
KateAndulaDoes the book cover TORCH infections like congenital CMV?
0 comments -
5 days, 7 hours agotina.a
Hi Emily!
At my 20 week ultrasound, we discovered that I had a rare kind of umbilical cord insertion— a kind of velamentous cord insertion called a furcate cord insertion, in which the umbilical cord actually separates into multiple strands before entering the placenta. We’ve only been able to find a little bit of data on this. Did you do any research about complicated cord insertions, and their impact on pregnancy outcomes? We’re at 29 weeks now, and the baby seems to be doing alright, but we’re worried about later pregnancy, labor and birth.
1 comments-
4 days, 21 hours agoMeganJB
I’m also curious about this one! We were told at the 20 week ultrasound we have a marginal cord insertion. Our doctor doesn’t seem especially concerned, which is reassuring, and she told us this diagnosis is becoming more common with better ultrasound technology. I’m similarly curious what this means for later pregnancy. It sounds like earlier delivery or complications with labor are possible, but I can’t figure out how likely. Even if I can convince myself not to be too worried, it would be nice to have a better idea if we should prepare for a more complicated birth, or a birth that’s earlier than expected.
0 comments
-
-
5 days, 7 hours agoalba.a
Is this a good book for people that already went through a pregnancy/birth? I’m currently trying to decide if I want to have another baby and after 4 years from my first child, I’m just starting to feel less triggered by my experience.
1 comments-
5 days, 6 hours ago Emily Oster
Emily OsterOur target audience for the book is people who had complications in a prior pregnancy or birth and would like help navigating or considering a second pregnancy.
0 comments
-
-
5 days, 6 hours agodclearwater
Do you cover the increased risk of complications that can come from pre existing conditions such as lupus or other chronic diseases? How do we think about our own personal risk profiles when considering a pregnancy?
0 comments -
5 days, 6 hours agotvdoctor
In your newsletter, you say, “Our hope is that it can be a starting point for normalizing discussions about these topics…” That feels off to me. It neglects the scores of parents who create and manage safe and supportive spaces for folks who’ve had miscarriages (like r/PregnancyAfterLoss). After my D&C, they sent me home with a giant packet of resources full of groups available to me.
For every person who mentions to me, “people don’t talk about miscarriage,” there are 3-4 others who barely need a cue to start talking about their experience with miscarriage. That’s “anecdata,” sure, but at this point, I think *people do* talk about miscarriage, but talking about it won’t prepare anyone for when it happens. Like any matter of grief. I knew when first trying to get pregnant that miscarriage is a real possibility. Almost every parent in my life had some experience with it. What they didn’t talk about? The decisions and the costs.
I had a missed miscarriage at 10 weeks, and immediately after finding out the news, I had to make very important physical and financial decisions. Pill or D&C? Question: How much does a typical miscarriage cost? It’s rotted, but I have to think like that because my out-of-pocket American insurance sucks.
And then the physical cost. It turns out, my body doesn’t respond to miscarriages well. I had/have raging chronic migraines and stopped ovulating consistently. I needed femara and a whole year just to see another positive pregnancy test. Question: What does recovery look like for different people and different miscarriage types?
I’d love to read about this on your site or in your book, which I’ll be picking up soon because I find myself in conversations about miscarriage *a lot.*
0 comments -
5 days, 6 hours agoFiona Clara
I was diagnosed with gestational diabetes at 20 weeks. In the GD chapter you mention that there may be some “clues” as to whether (1) you might have had undiagnosed pre-existing diabetes or prediabetes; or (2) your test results are purely because of GD. What are these clues?
1 comments-
5 days, 6 hours ago Emily Oster
Emily OsterIf you have other conditions which are associated with diabetes — notably, a higher pre-pregnancy weight — that would be a possible clue that a diagnosis could reflect an underlying condition.
Regardless: you should be screened for diabetes post-pregnancy, which will provide a complete answer to this concern.
0 comments
-
-
5 days, 6 hours agoLizK
I’d love to know more about how you got to the “50% of pregnancies will have a complication” stat. As someone who had a complicated pregnancy at the end it’s a sad, yet comforting thing to know (though I still hope it can improve).
1 comments-
5 days, 6 hours ago Emily Oster
Emily OsterIt’s an approximation but…
-25% first trimester miscarriage
-12% preterm birth
-Book discusses C-sections, about 33%
-Gestational diabetes: 7%
-Preeclampsia: 5%
-Growth restriction: about 10%You get to 50% pretty quickly on this.
But I agree I very much hope this improves.
0 comments
-
-
5 days, 6 hours agoBonnie425
I had a perfect, uncomplicated pregnancy that ended in stillbirth at 40 weeks. There’s no known medical reason for why our daughter died. Aside from extra monitoring, is there anything I can/should do differently if we get pregnant again?
1 comments-
5 days, 6 hours ago Emily Oster
Emily OsterI am so tremendously sorry for your loss.
As Nate writes about in the book, in nearly all cases having had a stillbirth doesn’t put you at an elevated risk for another one. You’ll be monitored more closely, both out of an abundance of caution and to help with anxiety. Usually delivery will happen earlier — at 39 or even 38 weeks — again, largely for mental health reasons.
0 comments
-
-
5 days, 6 hours agomurphnd
First, thank you so much for this book! I had a relatively easy pregnancy until my water broke at 29 weeks and my son was born by C-section at 30 weeks. I have two questions that aren’t covered in the preterm birth chapter: (1) Is there any data on the mother’s age affecting recurrence of spontaneous preterm birth? I was 41 when my son was born and will obviously be older than that if I get pregnant again. (2) During the C-section, the doctors discovered that the cord was wrapped around my son’s neck, which had been causing his heart rate to keep dropping. Is there any data (or even hypotheses) on that as a possible cause of preterm labor and the probability of recurrence?
0 comments -
5 days, 6 hours ago Emily Oster
Emily OsterOne reminder: we have a a story bank focused on pregnancy complications and loss from when I started outlining this project in 2022.
You can visit this here:
0 comments -
5 days, 6 hours agoLaura_v
Does the book cover risks for a subsequent pregnancy after a big hemorrhage due to placenta accreta?
0 comments -
5 days, 6 hours agomiaC
I was in the hospital this week for spontaneous preterm labor at 34.3 – very unexpected in an otherwise uneventful pregnancy. The doctor offered the option to get a steroid shot for baby’s lung development but said that recent studies do urge caution for babies that may be born full term due to an increased risk of developmental disorders (https://pubmed.ncbi.nlm.nih.gov/36001315/).
The cutoff for where they wouldn’t give steroids was 35 weeks… Dr. said it was a tough call but she would do it if it were her, so we opted to get the shot.
Since labor stopped naturally and I’m at 35.1, now every day that passes I’m worried that baby is developing a disorder. Can you reassure me that it’s better to be full term / at term with the steroid shot than preterm?
0 comments -
5 days, 5 hours agoOaklandReader
I just read your chapter on preeclampsia. I had severe preeclampsia with HELLP, and gave birth at 32 weeks. Things escalated so quickly. I was doing fine in my pregnancy and then went to the hospital after not feeling well and had the baby with emergency c section 12 hours later. The baby was in the Nicu for 6 weeks but is doing fine. I had been taking baby aspirin since week 12 because I was 35 at the time. The chart in the book suggests I would have a 50% chance of have severe preeclampsia or HELLP, preterm if I got pregnant again. Since I already took baby aspirin the first time, is there anything I can do to lower that risk? If not I will likely not feel comfortable having another kid.
1 comments-
5 days, 3 hours ago Emily Oster
Emily OsterOur best treatment here is aspirin –which lowers but does not eliminate this risk. Other than that, I’m sorry to say there is not much that could be done to decrease your risk in a later pregnancy. Having experienced this before you would be more aware of the warning signs, but in this case that may be of minimal help.
0 comments
-
-
5 days, 5 hours agoErin b
6 weeks PP I had an AV malformation in my uterus and was bleeding out. They embolized that part and saved my life. We are going through the process of seeing if we can have more kids. No one so far knows the data for successful second pregnancies. If you have a malformation, is the whole uterus like that or is it only the one spot that we embolized so it’s done? We can’t find any answerd on AV malformations. I don’t want to die.
0 comments -
5 days, 5 hours agoslcdm
hi! thanks for all you do. my daughters heart rate kept significantly reducing with each contraction after the epidural which led to urgent c section, an HIE moderate scare with very low apgar/hie scores and nicu cooling process (no other issues in pregnancy and no answers from c section—no obvious cord or placenta issues but we are waiting on placenta testing). my husband is pretty adamant it all started with epidural and i have seen infant duress as a side effect of epidural. is this a one off or should i have a second, should i be concerned about the epidural effects round 2? daughters mri was clear after cooling process so were very grateful.
1 comments-
5 days, 4 hours agocarolineclairemann@gmail.com
I was diagnosed with GDM during both my pregnancies and became rather obsessive about tracking my blood sugar, avoiding carbs, compulsively exercising etc. Thankfully both my girls were healthy, normal birth weights and my A1C is normal. I worry a lot about my future risk of diabetes and their risk of developing it in the future. I’ve read statistics with wide ranges on this and my doctors seem pretty unconcerned but the wellness space is rife with insulin resistance scares. Is my dear founded? Is there anything that can be done to reduce the risk of this for my daughters and me other than exercise and maintaining a balanced diet?
0 comments
-
-
5 days, 4 hours agokatherinepg
Diagnosed with complete placenta previa @ 20 week scan. Hospitalized from 32-35W due to hemorrhage & delivered @ 35W via C-section where accreta was discovered. Able to remove all but 3 pieces & managed bleeding via Bakri balloon and Uterine Artery Embolization. PPH at 4 weeks PP. Finally resolved 3mos PP via hysteroscopy; tests after showed minimal scar tissue.
So thankful doctor preserved my uterus. What are my chances of recurrence of previa and accreta?
0 comments -
5 days, 4 hours agoVictoria
I haven’t read this book yet but I look forward to it! Any disucssion included of how long after a male has chemo, his sperm is safe to conceive?
0 comments -
5 days, 4 hours ago Margaux
MargauxIs the book about unexpected things that can happen, or how to cope after it happens? I had a difficult birth and nearly 2 years of heavy bleeding until a fibroid was discovered/diagnosed as the issue. I find myself still navigating post-partum issues and emotions.
1 comments-
5 days, 3 hours ago Emily Oster
Emily OsterIt’s about both — but the focus is on how to navigate a future pregnancy after complications.
0 comments
-
-
5 days, 4 hours agoat468@cornell.edu
I have been trying for a second baby. On Month 5 I got pregnant and had a miscarriage week 5. My doctor said it was a chemical pregnancy and didn’t do any further testing. I would like to continue trying. I am 44 years old turning 45 this month. The data out there is pretty hideous as far as pregnancies after 40. I had a successful pregnancy at 43 to term. My question is should I just keep trying or try IVF or other fertility treatments. Also thank you so much for all your books. I read them all!
1 comments-
5 days, 3 hours ago Emily Oster
Emily OsterI am so sorry for your loss.
You’re right that the data is tough on pregnancies as we age past 40. Miscarriage rates increase, especially early miscarriage, since chromosomal abnormalities become more common. Certainly at this stage talking to a reproductive endocrinologist is likely a good idea — they can give you a much better individual sense of whether you are a good IVF candidate.
0 comments
-
-
5 days, 4 hours agolndemery
38 and trying to get pregnant again. Took me awhile to get pregnant with my last baby (maybe PCOS, but they aren’t sure). Will this book be triggering for me if I read while trying to conceive or am pregnant? I had a ton of miscarriage anxiety last time.
0 comments -
5 days, 3 hours agomaggiebean
While on holiday abroad, I experienced several gushes of fluid and was diagnosed with PPROM at 22 weeks, hospitalised for a week and on bed rest for a month. Thankfully I did not go on to lose any more amniotic fluid, and eventually returned home where I was monitored more closely. After initial talk of early induction, another doctor concluded around 8 months I had been misdiagnosed and probably did not have pprom to begin with. I went in to have an elective C-section at ft. However, I’m convinced that my membrane did rupture, but that the tear healed itself. I’d love to have another child but I’m terrified of this happening again and if pprom was confirmed would not want to try for another pregnancy. Would this book provide guidance on how to approach such a discussion with my doctor to better understand the odds & risks?
0 comments -
5 days, 3 hours agoKaeley
I had a miscarriage at about 10 weeks, then a pprom at 21 weeks (no known reason although I did have off and on spotting throughout the pregnancy) then a full term pregnancy that ended in an emergency c section due to my baby not tolerating contractions. We are hoping to have another baby but I want to make sure there are no unknown underlying issues before trying again. Are there any specific tests/questions I should request from my doctor before getting pregnant again? Is pprom in second trimester covered in the book?
0 comments -
5 days, 3 hours agoLjohnson1987
Hi Emily. I’ve so appreciated how informative your books are and the way it empowered me in my decision making during and after pregnancy. That said, after having 36 weeks of a perfect pregnancy, I felt bad and SO thirsty. Not sure I will ever have an explanation for this but at 38 weeks and 6 days, while in labor, I was diagnosed with preeclampsia with sever features (liver and kidneys/never had high blood pressure). After birth I was given magnesium which to me was more traumatic than the preeclampsia diagnosis. I don’t remember anything during this time. I’m wondering if you could explain more about magnesium as the information I find is not helpful. My understanding is that it brings your risk of seizure from already very low to barely lower. If I have a another baby and have preeclampsia again, I would like to decline this as not only did it make me feel terrible, not remember the first days of my baby’s life, but I also believe it is the reason I couldn’t breastfeed (info on this seems limited but seems like a real thing). Would love to know what data you have regarding magnesium. Thank you!
0 comments -
5 days, 3 hours agoEjwaves
I tried scrolling through all the questions but has anyone asked about shoulder dystocia? I have a suspected big baby and I’m nervous
0 comments -
5 days, 3 hours agoChrissy
I just had a MMC discovered at 19 weeks. Baby measures 18 weeks. All genetic testing came back normal as did the APS clotting testing I requested. My doctor says it was “bad luck.” Does the book cover how to proceed with a future pregnancy? I am so scared of experiencing this twice.
0 comments -
5 days, 2 hours agoBeba
Hi Emily,
Thank you for taking on this work and being a resource to us. I had monochorionic-diamniotic twins and many placental issues during the pregnancy- vasa previa, IUGR of 1 of twins, and ultimately severe sudden preeclampsia with emergency c section at 30w. My understanding is this was all related to twins, but do you know of any data of how this may affect risk of preeclampsia or other placental problems in subsequent pregnancy?
Thanks in advance for your help!0 comments -
5 days, 2 hours agomaryandw
Hi! After my second pregnancy, I had a PP hemorrhage and retained placenta that was about 90% removed with a D&C three months PP. It wasn’t all removed since the bleeding was getting heavy and my dr was worried about having to do a hysterectomy if it continued. I still have spotting about a year later.
We’d love another child in the future. Do you have any intel on getting pregnant again, with retained calcified placenta still present in the uterus?
0 comments -
5 days, 1 hour agoTiffany B.
My son was born at 36w and at 4lbs 10oz. I had a healthy pregnancy but clearly I had IUGR. He’s 5 now and is only in the 10th percentile for growth. What’s the data around long term growth for a premie that also has IUGR? Thanks!
0 comments -
5 days, 1 hour agoKatKLeaf
Do you touch on Hypoxic Ischemic Encephalopathy (HIE) or other forms of severe birth injury in your book? My first child had an HIE event and, while I did end up having a second child a few years later, some parts of her birth were eerily similar. For both, my water broke before contractions, both had a low baseline HR & both struggled and with heart rate dips during contractions.
0 comments -
5 days agorosemary
Curious to better understand the pros and cons of bilateral salpingectomy. I’m having a C-section in the next month and am considering the procedure while my doctor already has me open. I love the idea that it greatly reduces my chances of ovarian cancer, but I feel like there are still a lot of unknowns around how this could interact with menopause. Any insights on this in the book?
0 comments -
4 days, 23 hours agoamanda k
I had a normal pregnancy until it ended in stillbirth at 39 weeks. After delivery, upon testing, it was noted that cause of death was umbilical cord accident. In addition however, we found he was small for gestational age <10th percentile although no diagnosis of IUGR was established during pregnancy. The placenta was also very small <3rd percentile. No one has been able to tell me for sure these related to the cord accident/stillbirth.
I’m currently pregnant and I’ve been seeing a MFM who suggested 37 week induction to prevent another loss. I’m currently scheduled for 37+2 day induction. I’m wondering if this is too early, and I should ask to delay. But I am also terrified of another loss. Wondering if you’ve come across data of subsequent losses after stillbirth, or the data on these early inductions.
Thank you.
1 comments-
4 days, 17 hours agoTessaM
I know nothing about data but wanted to say my first pregnancy ended in stillbirth at 35+5, cause unknown but best guess a cord accident. My MFM supported/recommended a 37 week induction for subsequent pregnancies. Our later daughters were both born at 37+2. One needed NICU time, one didn’t. Both are great now. No regrets – I was so anxious at that point, and I couldn’t shake the worry about how I’d feel if something went wrong again after 37. Best of luck in whatever you decide, and so sorry for your loss.
0 comments
-
-
4 days, 23 hours agoKHFordMomma
36/37 year old. IVF pregnancy (took 5 rounds of egg retrieval to get 3 PGT normal embryos, but just one transfer). Flu, Covid, and Sinus infection in 2nd trimester.
Baby was small at 20 week anatomy scan but my concerns were brushed off by MFM.
High BP at 24 week OB appt, so sent to hospital for “monitoring.” Scan done at the hospital showed absent end-diastolic flow in the umbilical cord, so I was admitted until delivery at 27w6d (fought high blood pressure the entire time-several rounds of magnesium, steroids for baby-and I was in and was kept longer after delivery because BP kept getting out of control).
Baby was born at 625 grams, so very SGA even for her premature birth.
All of this leads me to think I should get tested for APS, but what if doctors don’t think so because I technically didn’t have repeat miscarriages (because it is not for me to conceive naturally due to missing and blocked fallopian tubes)? Do I keep asking? Find another MFM (even though he’s the only practice connected to my delivery hospital of choice)?
Is it even safe for me to carry another pregnancy?
Thanks for this book!1 comments-
4 days, 1 hour agoErincevers
I had absent end diastolic flow causing severe IUGR, eclampsia and stillbirth at 21 weeks. Where do you live? I’ve consulted with two MFMs in NYC who both advised a reproductive immunology protocol for my current pregnancy to keep the baby (and me) alive. I’m happy to pass along their information if you’re interested/that’s appropriate here!
2 comments-
3 days, 20 hours agoRevMcInMama
I’d be interested! I also had absent end diastolic flow and FGR, just no BP issues. Until seeing this forum, I’ve hardly heard of any other moms having AEDF
0 comments -
3 days, 11 hours agoKHFordMomma
So sorry for your loss. I’m located in the DC suburbs. I’m definitely interested in finding out what your docs suggested and what your protocol is this time around.
1 comments -
3 days, 1 hour agoErincevers
Hello! I consulted with two reproductive immunologists, Alex Kofinas and Jonathan Scher. I found them both incredibly compassionate and encouraging. They agreed that a RI protocol could help me carry to term, in part because during my last pregnancy, the baby stopped growing immediately after I stopped taking prednisone at 16 weeks. My current protocol, which they mostly agreed on, consists of metformin, Lovenox, Tacrolimus, Plaquenil, Prednisone and intralipid infusions until 34 weeks. I hope this is helpful – I’m happy to discuss more. I will also get a cerclage at 12 weeks (lost my first baby when water broke at 16 weeks). I should caveat that I’m a whole 4 weeks 4 days today, so the proof will be in the pudding I suppose. Fingers crossed!
1 comments -
3 days, 1 hour agoErincevers
I also want to add that this protocol was devised after a LOT of testing and is highly individual so I ofc don’t mean to recommend that anyone just start taking these meds wily-nily- but I hope it might be a helpful starting point for conversations w a RI. Best of luck to everyone!
1 comments -
3 days agoErincevers
Sorry for all the comments. Forgot to add Neupogen injections and LDN also part of my protocol
0 comments
-
-
-
4 days, 21 hours agoMGK
Thank you for your book (all of them really)! I’m pregnant with my second after an emergency c-section with my first. I appreciate how the book lays out the different risks between repeat c-section and TOLAC (including those associated with a second emergency c-section). Trying for a VBAC is my preference (partly because I’d like to have another child and my mom had a very scary case of placenta accretia so increased risk there scares me). However, my doctors tell me that a repeat c-section is strongly recommended since it was less than 18 months from birth to conception. Two questions: Is there data to support the 18-month cut off? Are placenta complications (accretia or previa) hereditary? Thank you!
0 comments -
4 days, 20 hours agolauraelizabeth
I have the book but have only skimmed it so apologies if this is redundant. I’m curious how you think about elective c section after a traumatic birth. With my first birth I had a series of rare, serious complications (severe sulcus tears, peritoneal hematoma, sepsis). Every provider I’ve spoken with says they don’t think a c section is medically necessary but they’d offer it. How do you weigh the overall increased risks of c sections vs the psychological difficulty of another vaginal birth?
0 comments -
4 days, 19 hours agoRevMcInMama
I had growth restriction with my first daughter back in 2020 that got diagnosed at 36 weeks due to her femur measurement being under the 10th percentile. Everything else was normal and I was induced just before hitting 39 weeks with a healthy baby. With my 2nd pregnancy in 2023, because of my history, I had a growth scan at 27+4. I was again diagnosed with FGR with abdominal circumference lagging and elevated umbilical dopplers. I had an initial round of steroids and moved to weekly monitoring. At 30+4 we had intermittent absent end diastolic flow that led to a hospitalization for additional monitoring. Then I was discharged for twice-weekly monitoring. At 34+1 we had repeat absent end diastolic flow (50%) with dopplers more than double the 95th percentile for GA. That led to our daughter being born via c-section. After about a month in the NICU, she is our tiny but mighty little one. Neither case of FGR revealed anything in pathology of my placenta so both were unexplained.
In the FGR chapter, it noted that given the randomness of occurrence, it can be likely to have a subsequent pregnancy that is “normal.” Given a repeat occurrence with the additional complications of absent flow, would that change likelihood of recurrence? Does it mean my body just can’t grow a fully healthy placenta?
0 comments -
4 days, 19 hours agoAWS3122
My water unexpectedly broke at 35 wks and was also diagnosed with severe preeclampsia right after and ended up delivering my baby 12 hours later. Both me and my baby have luckily been totally fine 2+ years later. I would have loved to have read this book prior to getting pregnant again. However, I’m 7 weeks pregnant now and I’m concerned this book could be “triggering” and make me question if I should have gotten pregnant again after I’m already pregnant. Thoughts on this concern?!
0 comments -
4 days, 18 hours ago@tutortori
Hi Emily, Does the book discuss diastasis recti or hypermobility? What do you believe the ideal postpartum care should look like? For example, should pelvic floor physical therapy be automatically offered by ObGyns? Should pre- and post-natal massage therapy be covered by insurance?
For context, my births 4 years ago and 2.5 years ago both disabled me, and I still haven’t recovered a functional core (or normal exercise generally). The combination of hypermobility and diastasis allowed my spine and hips to “melt”/deform, causing excruciating pain and disability that went undiagnosed for months. Thank you.
0 comments -
4 days, 18 hours agoAmy Beth
After my second pregnancy, I was diagnosed with severe postpartum preeclampsia after delivering via planned c-section at 39 weeks. I’m nervous that this may happen again if I decide to have another child. Would delivering at 37 or 38 weeks decrease my chances of postpartum preeclampsia (assuming it doesn’t occur before then)?
0 comments -
4 days, 18 hours agoMaggie P.
Do you discuss the risks of future pregnancies after having preeclampsia? I had gestational hypertension with my first and preeclampsia with my second birth.
0 comments -
4 days, 17 hours agoCrob1
I hemorrhaged about 2-3 hours after giving birth due to retained placenta. It was a serious hemorrhage and an emergency, and they had to manually attempt to remove the retained placenta without anesthetic or pain relief, leaving me with serious trauma from the pain.
Two questions:
1. What is the chance in a second pregnancy that I will retain placenta again?
2. Can they do anything proactive to provide pain relief, were this to happen again? I’m so, so scared of experiencing that again.I went into birth so calm and excited and had a wonderful, empowering experience, up to that point. I think I want a second child, but I also am fearful that I will be panicking my entire pregnancy.
0 comments -
4 days, 13 hours agoDiabeetusFetus
Hi Emily!
I am currently in my second pregnancy with diet controlled gestational diabetes. In the book, it says there are good outcomes as long as blood sugar is “mostly normal”. What does that mean? How many times can your blood sugar spike before it actually becomes a concern? Trying not to beat myself up when something like an apple pushes me over the limit!0 comments -
4 days, 12 hours agoccs87
Do you cover chromosomal abnormalities in the book? Last year, I had a pregnancy that ended due to Triscomy 21, noted under “severe Down syndrome” due to my test results and soft markers that noted not carrying to term at 13 weeks.
I am pregnant again (11 weeks) at 36 y/o. Are there increased chances of chromosomal abnormalities since I’ve had one before and/or due to my age?
0 comments -
4 days, 5 hours agoTothehills
How does covid affect preeclampsia? Can paxlovid be taken during pregnancy? I had mild preeclampsia, got covid in December 2023, doctors advised against paxlovid and said I should just deal with the covid symptoms, my preeclampsia became severe within days, and I had to deliver at 35 weeks. Curious if this escalation could have been avoided or managed better. Thx!
0 comments -
4 days, 1 hour agoErincevers
Hello! I have had two difficult pregnancies that ended in 1) miscarriage at 16 weeks and 2) stillbirth at 21 weeks. In the second, I developed eclampsia – severe liver and kidney failure, extreme blood loss, critically low sodium and seizure. I’m pregnant for the third time and have a wonderful MFM who has me on an immunology protocol to try to prevent my body from rejecting the pregnancy. Do you cover these topics in the book? I’m so interested in reading it but given the PTSD I already carry w/r/t pregnancy, I’m not sure now is the right time. Thank you!
0 comments -
3 days, 8 hours agoMaria
Hi, does your book touch up on postpartum pulmonary embolism (estrogen induced caused by pregnancy)?
0 comments -
3 days, 7 hours agobekahandjosh
Why not give the steroid shot for lung development to all twin pregnancies?
My wife and I had a due date of 4/21 for our b/g twins. They moved us 4/8 since they don’t want twins going 40 weeks.
The doctor mentioned several times that we could do a steroid shot if preeclampsia symptoms appeared. This would help our twins’ lungs develop.
We ended up having preeclampsia set in and delivering on 3/13 (~6 weeks early). It was a relatively easy 20 days in the NICU (which I say because another set of twins born that day was life-flighted elsewhere). They’re home happy and healthy.
The only reason that we got the steroid shot is because we happened to come to the doctor’s on 3/11. One test was a bit high, so we pushed for the steroid shot just in case. We got the first dose that afternoon. It needs two doses and 48 hours to be effective. Early the next morning (3/12), we went to the hospital in labor. They gave us dose two that morning. Then, our twins are born after 24 (long) hours of laboring at the hospital.
We’ve been of two happy and sleep-deprived minds since. On the one hand, is there a chance that the steroid shot worsened preeclampsia? On the other, holding the early labor start constant, surely it would have been better to get the steroid sooner than we did?
So, why not just do the steroid shot for all twin pregnancies?
Twins tend to be small and come early. It seems like an excellent place to have a steroid shot planned for twin mothers. Just like mothers receive maternal vaccinations, they’d receive a steroid shot to help the twins. Or, mothers with signs of preeclampsia could have it. We had high blood pressure throughout our pregnancy, for example. But maybe there are risks we weren’t aware of then?
I’m looking forward to reading The Unexpected–we had plenty of unexpected events in our pregnancy. Your other books helped handle those uncertainties and make our own educated calls.
0 comments -
3 days, 6 hours agoTwinmomA&T
Is the unexpected a good read for me even though I feel like I’ve processed my labor trauma and I don’t plan to have more kids? I love everything you write, but also am unsure if I should dive back into that world!
0 comments -
3 days, 3 hours agoeben
Hi! It seems the target audience for folks who have had complicated births. I love your books and was about to get this one, I feel like I need all the information, but then I realized some the content I was seeing on IG etc was actually triggering anxiety for what could happen, people’s stories of late pregnancy loss etc (I am going to be a FTM, currently 31 weeks pregnant, with no complications so far…). Is there any value for a FTM who so far has had a healthy pregnancy, or should I skip for now?
0 comments -
3 days, 2 hours agoLucy
Do you discuss VACTERL syndrome at all in the book? My son was born at 36 weeks with TEF/EA, hypospadias, and a persistent left superior vena cava. He’s mostly thriving now but our first few months were hell — 5 weeks of it spent in the NICU — and also, we weren’t prepared for it really. The only real indicators when I was pregnant (for TEF/EA) was polyhydramnios, which didn’t become excessive until two days before I went into labor. Phew, in all this, my question is, how does having one baby with VACTERL syndrome impact the likelihood of having another?
0 comments -
3 days agoRayna
Thank you for bringing the conversation about pre-eclampsia to light- I had it pre and post-delivery- and am now contemplating baby #2. Both times being treated with magnesium- in your research, did you come across any data about the medical impact of magnesium on mom/ baby or other options? What is the ROI? (personally, it was horrible, impacted bonding and breastfeeding but guess I would feel better knowing there isn’t another option or the pros outweigh the cons)
0 comments
- You must be logged in to create new topics.
Log in
Username
Your automatically generated username is currently set to: .
Your username will be publicly shown when you comment. Before posting, please update it in your
account settings..




 Back to Topics
Back to Topics
 120
120
 share
share