As a midwife, I love getting the chance to see a mom whom I’ve followed throughout the pregnancy for a postpartum visit. In addition to trying to sneak in a cuddle if she’s brought the baby (can you blame me?), I can’t wait to hear how she’s getting along. Whether or not I was the attendant at her birth, I want to know how she felt about it. Did it go how she expected and wanted? Is she feeling disappointed or confused about anything? Does she feel like her body is recovering as it should? How is the family adjusting to the new little person?
The purpose of this visit is to give moms a chance to unpack their postpartum experience with a seasoned midwife or doctor who can act as a trusted advisor during the journey.
But sadly, nearly 60% of new mothers skip the recommended postpartum visit. It’s easy to understand why. Leaving the house with a newborn is hard! In the U.S., our healthcare system doesn’t make it much easier. Home visits and telehealth options for postpartum care are often limited, so moms are expected to pack up their tiny baby and giant diaper bag, travel across town, and then sit in a waiting room for what could end up being a very short, impersonal, perfunctory visit.
On top of that, many mothers are juggling other young children, planning the new baby’s many medical visits, or even preparing to return to work due to limited maternity leave. During such an overwhelming time, it’s understandable that one more appointment, especially if you’re feeling fine, just doesn’t feel worth it. Frankly put, a lot of moms just don’t see the value of this visit.
But skipping it can mean missing important opportunities to care for your own health. Given all the emphasis on newborns, moms’ health often takes a back seat. Yet we know that about two-thirds of maternal deaths happen in the postpartum period, when complications and emotional challenges can arise, and that postpartum depression is on the rise, now affecting approximately one in every five moms.
Even mothers with pregnancy-related risk factors that carry important long-term health implications, such as gestational diabetes or hypertensive disorders of pregnancy, often miss out on the recommended follow-up care and screenings. The postpartum visit is an opportunity to talk about these issues early, get support, and focus on your own healing.

When does this postpartum checkup happen?
Traditionally, the standard of care for obstetrics was to do a postpartum checkup at six weeks. While that number might seem arbitrary, it probably comes from the observation that, by six weeks, the uterus has usually returned to its pre-pregnancy size, bleeding has slowed or stopped, and incisions or lacerations have mostly healed. For many providers, this was the point when it felt safe to give the “all clear” to resume normal activities like sex and exercise.
But in reality, healing from pregnancy and childbirth is a physical and emotional journey that unfolds over months or even years. Recognizing that a single six-week visit can’t meet the complex needs of all postpartum women, the American College of Obstetricians and Gynecologists (ACOG), together with the American College of Nurse-Midwives (ACNM) and other professional organizations, recently issued new guidance called Optimizing Postpartum Care.
This updated approach reframes postpartum care as an ongoing process rather than a one-time appointment. It recommends that all mothers have contact with a healthcare provider within the first three weeks after birth—or sooner if there are risk factors such as preeclampsia or a cesarean birth—and that a comprehensive, individualized visit take place between four and twelve weeks postpartum.
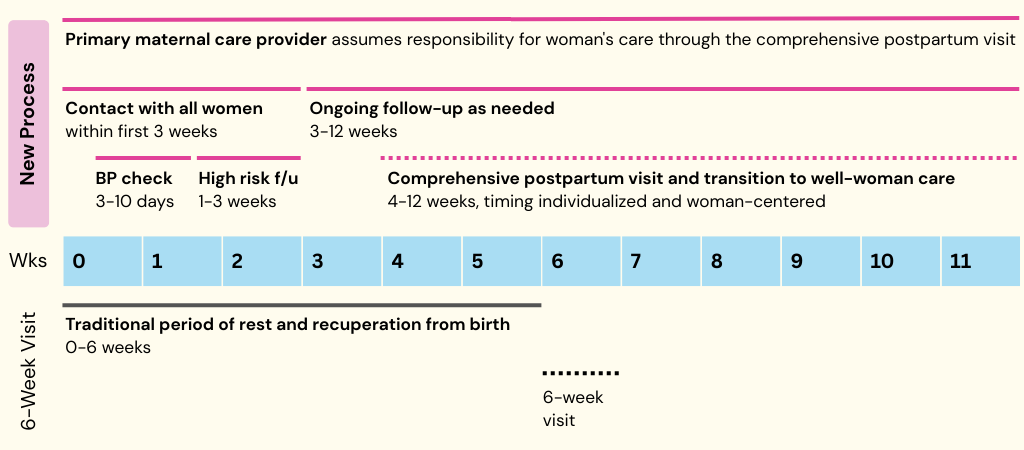
At my clinic, we’ve adapted these guidelines by offering all new moms a home visit with a nurse within the first three weeks, plus an in-person appointment if they had preeclampsia, a C-section, or a third- or fourth-degree laceration. We now schedule our comprehensive postpartum visits at four weeks instead of six to better care for moms at a time when they still have a lot of questions.
How to make the most of your appointment
This is an important appointment, and it’s typically pretty quick. To get the most out of your postpartum care, below are some areas to reflect on and discuss with your provider.
Keep in mind that this is not an exhaustive list! You should definitely feel free to ask questions tailored to your own needs and experience. Even touchy questions about sex, weight loss, and relationships are on the table. No matter how embarrassing or personal your questions feel, or how gross you think that picture of the giant blood clot is, chances are your doctor or midwife has seen it before.
Given the time crunch experienced by a lot of providers during a typical clinic day, it’s a good idea to do the following to prepare for your visit:
- Make a list of your top three concerns—the things you most want to talk about
- Bring along any medications you’re taking, as well as blood pressure or blood glucose logs
- Plan to ask for any referrals you need (pelvic floor therapy, mental health, lactation, etc.) early in the visit
Physical recovery and well-being
How are you healing from delivery (vaginal lacerations, C-section scars)? Any ongoing pain, bleeding, or signs of infection? Any bladder or bowel leakage? If so, a referral to pelvic floor therapy can make a huge difference. If you had gestational diabetes or high blood pressure, your provider may check your blood sugar or blood pressure to ensure they’ve returned to normal.
A 75-g oral glucose tolerance test is recommended at 4-12 weeks postpartum for anyone who had gestational diabetes in pregnancy. A CBC may be recommended to moms who had anemia during pregnancy, or who lost a lot of blood due to a postpartum hemorrhage. Further appointments to check on blood pressure may also be warranted.
Mood and emotional well-being
Has any aspect of your birth been traumatizing or hard to accept? Are you feeling isolated and alone? Do you have friends and family available to help? If you’re concerned about depression or anxiety in the postpartum period, do you need a referral to talk to a therapist or psychiatrist? Are you considering medications, such as an SSRI? Are you involved with any support or mom groups?
You may be given a screening tool to complete, such as the Edinburgh Postnatal Depression Scale (EPDS), and advice may be tailored to your responses.
Adjustment to infant care and feeding
Are you getting enough rest to function day to day, or is exhaustion starting to affect your quality of life and your ability to safely care for your baby? What support or resources do you have to help you get through this stage — whether that’s a partner, family member, or even a nap helper for a few hours?
How is the feeding going? If breastfeeding, is it painful? Have you met your breastfeeding goals? Is any lactation help needed? Are you happy with your decision and experience around feeding choice?
Family planning
Have you and your partner thought about how many kids you’d like to have and how much space you’d like to put between them? Are you interested in starting a birth control method if you haven’t already? If so, which methods would you like to learn more about?
Sexual health and relationship changes
Do you feel ready to resume sexual activity (generally not advised until after six weeks, but some people feel ready sooner)? Have you noticed changes in your or your partner’s libido? Are you struggling with body image or worried about relationship strain?
Chronic disease management
If you had any conditions preceding the pregnancy or complications during it, have you been able to follow up? Do you need help transitioning into primary care or a referral to see a specialist? Do your medications require adjustment now that you’re not pregnant?
It really helps to bring your medications and blood pressure logs if you have them!
Health maintenance and preventative care
Are you due for a pap smear? Any immunizations? Mammograms? When should you come back for your next exam?
Social determinants of health
Do you feel safe in your relationships? Do you have concerns about intimate partner violence, financial stress, housing instability, or access to care? Would you benefit from a social work referral to know what resources are available?
Closing thoughts
The best way to get the most out of your postpartum care is to remember that caring for yourself is part of caring for your baby. The reality is that when you have a new baby, life doesn’t go back to how it was before. Your body, routines, and priorities shift in big and small ways. Your postpartum journey deserves the same attention and continuity as your pregnancy, and you’re not supposed to navigate it alone! In addition to family and friends, your midwife or doctor can be an important ally.
The bottom line
- Official recommendations for postpartum care have shifted from a single six-week checkup to an ongoing, individualized process starting within the first three weeks, with comprehensive follow-ups between four and twelve weeks to better support physical and emotional recovery. (Although not all practices will follow this model.)
- Come prepared for your appointments with your top concerns. They’re typically pretty quick appointments, so getting organized in advance will help you make the most of your time.
- Postpartum care works best when you prioritize your own recovery alongside your baby’s needs, recognizing that your body, routines, and support system all need attention, and you don’t have to navigate it alone.





















Log in