Mastitis. If you’ve had it, the word itself prompts a reaction. When I mentioned the topic in our ParentData Slack channel, one team member commented, “Just the thought of this gives me a fever.” For me, the salient memory is adhering to the advice to feed the baby first from the affected breast. I love my son, but I did not love him at that moment.
For those who have no idea what I am talking about, here’s a quick overview. Mastitis, in general, refers to a condition in which the breast is swollen, hot, and painful. It can occur outside of breastfeeding but is most common during that period, when it’s referred to as “lactational mastitis.” Lactational mastitis occurs in something between 2% and 10% of breastfeeding women and is part of a much larger continuum of related discomforts.
I’m going to talk today about guidelines for treatment from the Academy of Breastfeeding Medicine (ABM), and in these guidelines they have an excellent graphic, which I’ve included below.
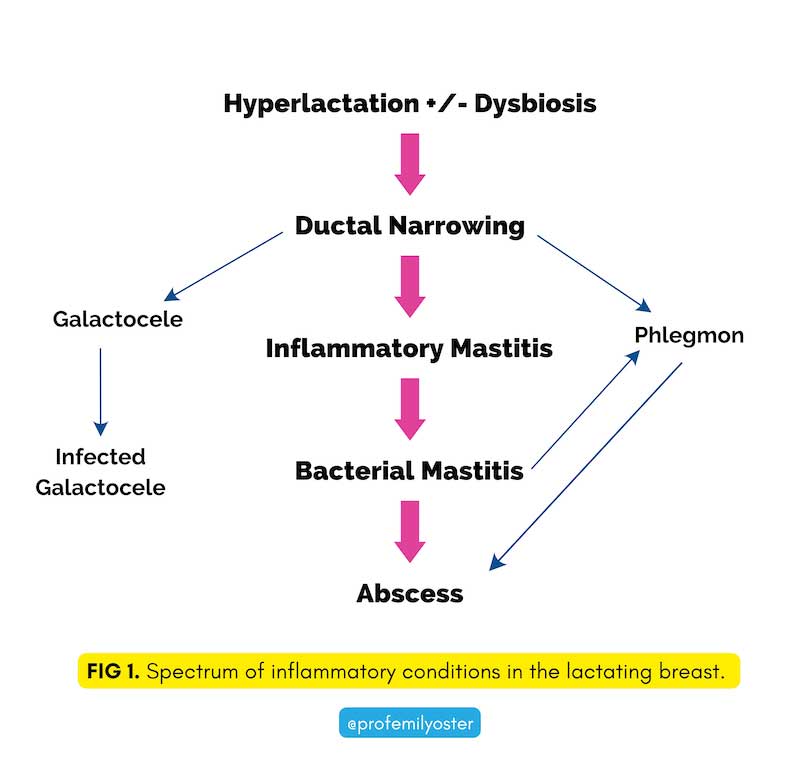
Some of the words here are a little jargony (“hyperlactation” = oversupply; “dysbiosis” = bacterial overgrowth), but what I like about the graphic is the illustration of the continuum.
Mastitis often starts with a combination of an oversupply of milk, and bacterial growth. Oversupply of milk can occur for various reasons — it is common in the early weeks of breastfeeding, during weaning, or at any time when the cadence of nursing changes and your supply needs to adjust. The oversupply can lead to milk stagnating in the breast, which can cause bacterial growth. The excess bacteria and milk can lead to a narrowing of the milk ducts, which can then progress to inflammatory mastitis. That can then progress to bacterial mastitis or (rarely) to abscess.
When mastitis progresses to the later stages, it can lead to systemic symptoms — fever, fatigue. In these cases, there is widespread agreement that it is necessary to treat it with antibiotics, and antibiotic treatment is effective in nearly all cases. And it is completely fine to continue to nurse while on antibiotics.
Important note: Please do not be anxious or reluctant to ask your doctor about this. Do not just suffer in silence!
What this image and discussion make clear, however, is that there are stages before that point at which it may be possible to reverse course. Mastitis, in early stages, can and often does resolve on its own. To enhance that possibility, women are typically prescribed what we might call “supportive care.”
We can divide the supportive care advice into two parts. The first is what we might call the “non-specific” or “obvious” part. This includes advice like “drink fluids and rest” (easy to say, harder to do with a baby), take ibuprofen or Tylenol for pain, and avoid wearing tight sports bras.
The second is advice that is more distinct to the breast. Looking over the popular Mayo Clinic website and the advice in UpToDate, a website for doctors, we see four key recommendations:
- Apply warm compresses to the breast or take a warm shower.
- Breastfeed frequently, starting with the affected breast.
- Use a pump to express milk between feedings.
- Massage the breast area.
This has been the standard advice. It is the advice I got when breastfeeding. However: in 2022, the ABM has come out with guidelines, and, on these particular pieces of advice, they pretty much say the exact opposite. Here is my summary of their version:
- Apply ice to the breast. Warm compresses might make things worse.
- Continue to breastfeed, but do not favor the affected breast; in some cases, use only the unaffected breast.
- Minimize breast pump usage; do not “pump to empty” the breasts.
- Avoid deep massage of the breasts.
I had a feeling a bit like the change in allergen advice — this does not just walk back the existing recommendations; it literally says the opposite. The ABM says the existing advice might make things worse! Naturally, I got curious about what changed. Was there some big study? Did our understanding of breast biology alter in some way?
My attempts to figure out the answer to that led me down something of a guideline rabbit hole, or more like an infinite guideline loop. For example, in the UpToDate entry on this topic, they provide a number of citations for their advice. Those citations, though, rather than containing evidence on particular recommendations, are just other restatements of the advice. These statements cite back to other statements, and so on.
In several cases, the guidelines I found linked back to earlier guidelines from the ABM. But those guidelines were superseded by the 2022 guidelines that were released. So … did that mean that actually everyone agreed with them? It was unclear.
Beyond this, when there were studies linked, the evidence was underwhelming. For example, in the 2022 guidelines, the authors state: “The use of warm showers and antipyretics [fever-reducing medications] did not improve mastitis outcomes in a randomized controlled trial.” This statement seemed quite compelling to me, and is perhaps the strongest direct refutation of the older advice. When I went to the citations for this claim, though, I found a randomized trial of acupuncture for treatment of mastitis. The trial rejected the value of acupuncture, but I didn’t see anything on showers.
Searching through the text, I found the evidence in support of the warm shower claim. One of the groups took more warm showers than the others and didn’t have their mastitis resolve any more quickly. This is weak evidence — it certainly isn’t randomized — and the samples in this paper are small (200 women in total over three treatment groups).
In the end, I found it difficult to find compelling data to support either side of any of these claims. (More on my feelings on that travesty at the end of this piece.)
This is slightly different, however, from saying there is no information to support any of the claims. The Academy of Breastfeeding Medicine article makes a weak case for their changes based on data, but a much stronger one based on logic.
As I noted at the top, mastitis is part of a continuum that often begins with an oversupply of milk and ductal inflammation. The logic in the article is simple: if you want to address the problem, you need to address these causes. This means downregulating supply, especially from the affected breast, and reducing inflammation. It is these observations, rather than experimental data, that point to the conclusions.
Hot versus cold for treating mastitis
Any kind of topical temperature change on the breast would be designed to treat inflammation. In general, inflammation is more often treated with ice rather than heat. This is a generic statement about all inflammation (it’s why I have these ice shoes to put on after I run), but we can see why it would apply here too. If you want to treat inflammation, ice is the initial go-to choice. If you do not want to put ice directly in your shirt, there are breast-specific cold packs.
Which breast? Pump versus not?
The advice about which breast to start on and whether to pump are intimately related to the issues of oversupply.
To the extent that oversupply of milk contributes to mastitis, treating it will involve lowering supply. Breast milk supply responds to demand. If you nurse and pump more in general, your body learns you need to produce more milk and makes more of it. Similarly, if you nurse and pump more on one side, that side will be more active. This is something you may be familiar with if your child has a favored breast. One of my kids vastly preferred to nurse on the right side, and it led to a very lopsided look (it mostly got better).
By extension of this theory, though, if you take a breast that already has an oversupply and you encourage more supply, you might make the problem worse. Much of the standard advice has this feature. Encouraging people to start nursing on the affected side will increase production on that side. Pumping between feedings, or “pumping to empty,” also generates more supply.
In contrast, starting nursing on the other side and avoiding or limiting use of the pump will help the breast regulate. This is a bit of a balance. Especially with an engorged breast, completely ignoring it will also be very painful. An approach of “pumping (or hand-expressing) to comfort” (rather than to empty) may be a way to generate the right feedback without stimulating supply.
Massage for breast pain relief?
Massage is actually the trickiest part of this. There is general agreement that very light “sweeping” massage can be effective and relieve pain. However, in some cases people will more aggressively massage in an effort to remove a perceived milk “plug.” This will not work, though. Mastitis isn’t caused by a particular stuck piece of milk in a tube. The breast has many, many ducts, and they get inflamed, but not plugged-up. As a result, aggressively massaging to remove a milk plug doesn’t make sense.
And, further, when you already have inflamed tissue, deep massage can possibly make things worse, by increasing the inflammation and damaging the tissue.
In summary
Based on the logic of breasts and breastfeeding, these updated guidelines make some sense.
Most key and important seems to be the guidance on supply. If you take nothing else from this discussion, it should be that stimulating more supply in the affected breast is not a good idea.
Beyond that, what I took from this was a feeling of frustration. A huge share of breastfeeding women will experience some form of inflammation or mastitis during their breastfeeding journey. All of these people are looking for relief, and we should be giving them advice based on evidence. Despite this: the data is so limited that literally people are getting the exact opposite advice, depending on who gives it.
My call to action here, then, is for someone to do a randomized trial. I do not think this would be all that hard. Recruit people with mastitis, randomize into different protocols, figure out if ice really works better than heat. Figure out the right protocol to relieve engorgement without generating more oversupply. See if it is possible to improve knowledge about massage. I hope someone will do this. If you need help recruiting a sample, please let me know.
Final note
If you want more on this, or to understand it all better, I highly recommend the detailed description of the updated guidelines, which you can find here. It contains a number of extremely helpful visuals, along with a fairly clear discussion of the underlying medical issues.
Community Guidelines














